Traumatic brain injury (TBI) is one of the leading causes of death and disability worldwide. For survivors, the long-term consequences can be devastating, from impaired movement and cognition to behavioral and emotional changes, deeply affecting not only patients but also their families. Despite advances in rehabilitation, existing treatments remain limited in helping the brain recover from lasting neurological damage.
Against that backdrop, bone marrow stem cell therapy is emerging as a promising new approach in the field of regenerative neurology. Globally, there have been only a few clinical studies evaluating the use of bone marrow mononuclear cell (BMMNC) infusion for patients with post-TBI complications; particularly in Asia.
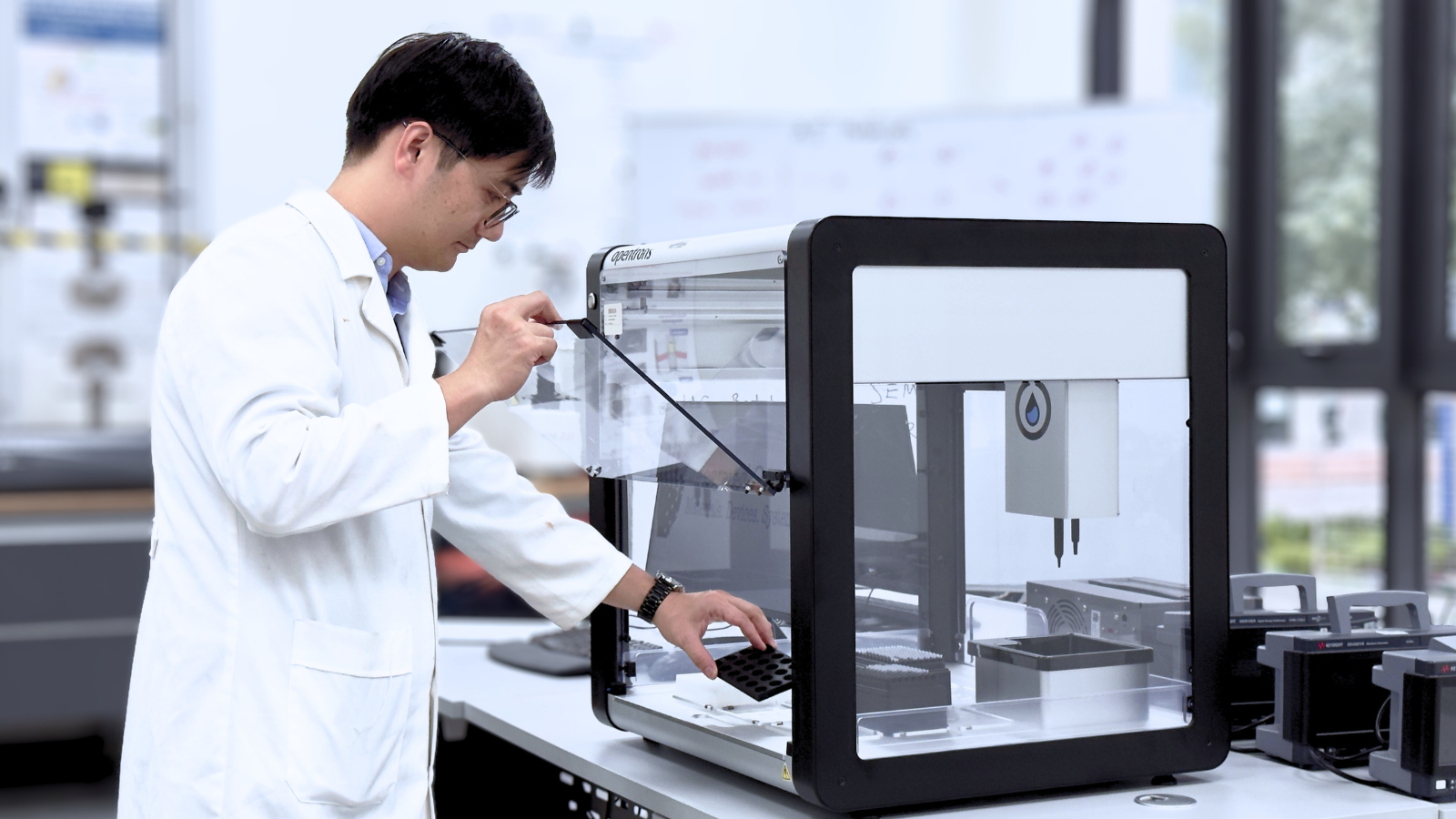
A recent clinical trial led by the Vinmec Research Institute of Stem Cell and Gene Technology (VinUni), in collaboration with Vinmec Healthcare System, Hanoi Medical University, and the National Rehabilitation Hospital, has just been published in Brain Communications, one of the world’s leading neurology journals, published by Oxford Academic (University of Oxford).
This matched-control clinical trial involved 50 patients living with long-term neurological impairments after TBI. The intervention group received two intrathecal infusions of bone marrow mononuclear cells, six months apart, combined with rehabilitation therapy, while the control group received rehabilitation alone. All patients were followed for 12 months to assess safety and effectiveness.
The results were encouraging. The therapy proved safe, with no serious adverse events reported. Minor side effects, such as temporary pain or dizziness, resolved on their own. Patients receiving stem cell therapy showed notable improvements: average motor scores (movement ability) increased by 4.3 points (p = 0.02), cognitive scores by 1.7 points (p = 0.009), and quality of life, both physical and mental, improved significantly (p < 0.05). These p-values confirm that the improvements were statistically meaningful, not random.
Beyond the statistics, MRI scans revealed visible structural recovery in the brain, while PET-CT imaging, which measures brain metabolism and activity, showed significantly higher neural activity in treated patients.
More importantly, behind each statistic is a human story: a first step after months of immobility, a regained smile from someone who once lost hope. Many patients who had been unable to walk or work have regained their independence after treatment.
This study highlights the potential of regenerative medicine, where stem cells may hold the key to repairing brain damage once thought irreversible. It also demonstrates Vietnam’s growing capability in clinical research and translational science, led by academic medical centers like VinUni–Vinmec, working together with Hanoi Medical University and the National Rehabilitation Hospital.
The research stands as a testament to the power of academic–clinical collaboration in Vietnam. It marks an important step toward bringing “made in Vietnam” stem cell therapies to the global stage. It reminds us that the mission of science is not only to heal, but to restore hope for those in search of a second chance in life.